A Common Virus Causes Cancer, but Most Americans Are Clueless About It
The human papillomavirus (HPV) is a major source of cancer that’s now almost entirely preventable through vaccination. But sobering research out today shows that Americans are largely in the dark about HPV and its many health risks, much less the HPV vaccine.
Researchers at the Medical University of South Carolina conducted the study, which examined nationally representative survey data. A third of Americans don’t know that the virus exists, they found, while most who do know are still unaware it can cause more than one type of cancer besides cervical cancer. People in certain regions of the country, particularly Midwest and Southern states, were even less aware of HPV, which likely helps explain why vaccination rates are lagging in these areas, the researchers say.
“Some of these states have the lowest HPV vaccine coverage in the nation, which could be a reason why we are observing these differences,” lead study author Ashvita Garg, a public health researcher at MUSC, told Gizmodo.
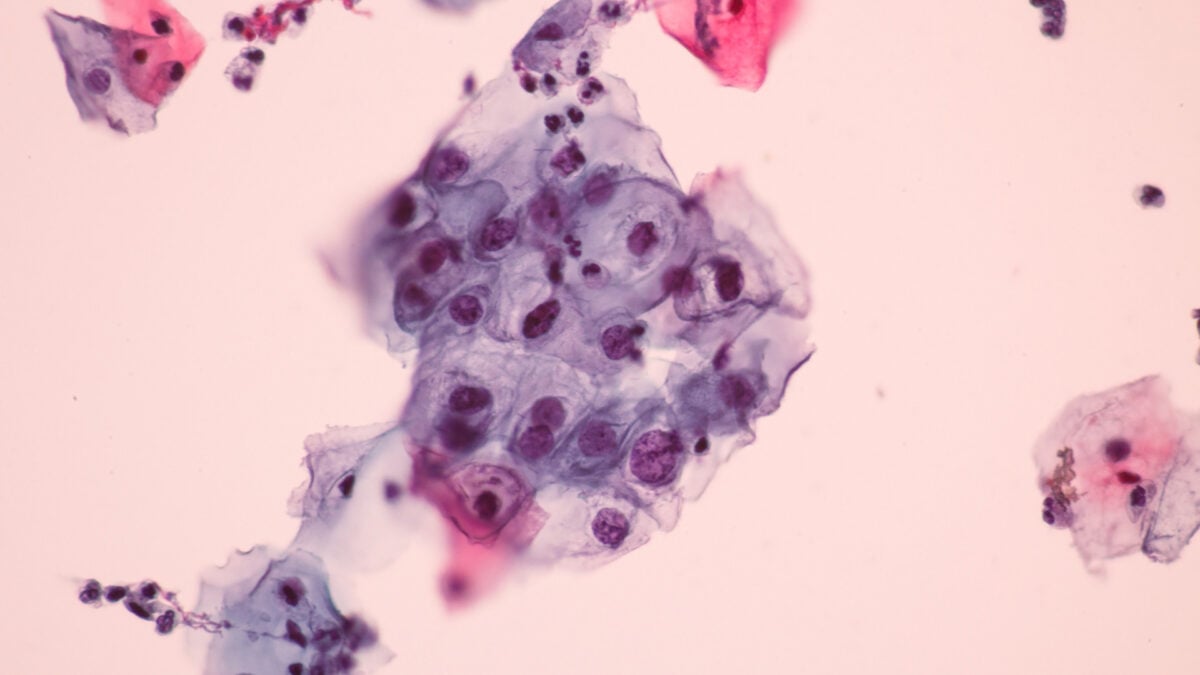
There are over 200 different types of HPV, which is spread through skin contact (including sexual contact), and HPV is the most common sexually transmitted infection worldwide. Some types are low-risk, only causing unseemly but harmless warts along our skin or genitals. Other high-risk types can linger in the body and cause damaging changes to normal cells that raise their risk of becoming cancerous.
HPV is the leading cause of cervical cancer, accounting for nearly all cases. But high-risk HPV infections are also primarily responsible for several other kinds of cancer, including vaginal and vulvar cancers in women, penile cancer in men, and oral cancer in both men and women. In fact, HPV-related oral cancer is more common in men than it is in women. All told, about 40,000 HPV-caused cancers occur annually in the U.S.
Today’s vaccines can prevent up to nine different high-risk types of HPV, but the vaccination rate remains relatively low in many parts of the world, the U.S. included. The researchers sought to better understand just how aware people are about the virus and the value of vaccination.
The researchers studied data from the Health Information National Trends Survey (HINTS), a project run by the National Cancer Institute that regularly measures Americans’ knowledge of health and cancer-related information. Their sample ultimately included almost 23,000 responses collected between 2017 and 2022.
Based on the survey data, around 34% of Americans nationally were ignorant about the existence of HPV, and 37% were ignorant about the HPV vaccine. Of those who did know about the virus, 71% didn’t know that it can cause oral cancer, and 28% didn’t know it caused cervical cancer. Ignorance of HPV and the vaccine was especially high (over 40%) in seven states, including Kansas, Nebraska, and Illinois in the Midwest, as well as Mississippi, Arkansas, and Alabama in the South. These same states have some of the lowest HPV vaccination rates in the country, and about 62% of all HPV-related cancers occur in the Southern and Midwestern U.S., the authors note.
“Additionally, the gap between awareness that HPV causes oral cancer was notably larger compared to the awareness that HPV causes cervical cancer, highlighting the undervaluation of the importance of HPV vaccination in males,” Garg said. The team’s findings were published Thursday in JAMA Oncology.
Some countries have already started to effectively eliminate cervical and other HPV-related cancers through widespread HPV vaccination, but the U.S. is still lagging well behind. Overall, only around 57% of American teenagers in 2023 received the HPV vaccine as recommended, well below the 80% target goal that health officials are hoping to reach by 2030. The researchers say that much more effort is needed to improve people’s knowledge of HPV and its dangers.
“Improving HPV awareness would require a multifaceted approach, such as public education campaigns, improving patient-provider communication, and community and school-based outreach programs,” Garg said.
Unfortunately, the federal government may not be so interested in HPV prevention these days. Robert F. Kennedy Jr., the current health secretary, has regularly spread misinformation about the HPV vaccine and even referred to Merck’s HPV shot, Gardasil, as the “most dangerous vaccine ever invented.”
All that said, Garg and her team at MUSC are still dedicated to improving HPV vaccine coverage in their neck of the woods.
“Beyond examining the HPV-related cancer burden and mortality, we are also investigating the uptake and delivery of HPV prevention modalities and understanding prevention behaviors across the US,” she said. “MUSC is also actively involved in public health outreach, particularly in South Carolina, where initiatives like the HPV Vaccination Van are helping to improve education and access to HPV vaccination.”



- CỘNG ĐỒNG
- News
- Tech
- Food
- Causes
- Personal
- Art
- Crafts
- Dance
- Drinks
- Film
- Fitness
- Παιχνίδια
- Gardening
- Health
- Κεντρική Σελίδα
- Literature
- Science
- Networking
- Party
- Religion
- Fashion
- Sports
- Αστέρια
- Xã Hội


